LUMS Electrical Engineering Faculty Proposes Affordable Non-invasive Glucose Monitoring
As of 2020, according to the International Diabetes Federation, 17.1% of the adult population of Pakistan, which is about 19 million out of 113 million adults, suffers from diabetes. According to the Institute for Health Metrics and Evaluation (IHME), an independent global health research centre at the University of Washington, diabetes was ranked in the top ten causes of death in Pakistan in 2017.
Diabetes is a disease, which impairs the body’s ability to produce insulin or hinders the effective use of insulin in the human body. Insulin is a hormone that regulates our blood glucose levels by allowing our bodies to either use or store the sugar (glucose) from carbohydrate enriched foods that we consume. This disease spares no one, it is prevalent in children, the youth, adults, and pregnant women. Untreated, it could lead to multiple organ failure eventually resulting in death.
Dr. Wala Saadeh from the LUMS School of Science and Engineering’s Electrical Engineering Department came up with the idea of developing an affordable and non-invasive blood glucose level monitoring device. The inspiration for the idea came when she met a woman and her diabetic child at the airport, Dr. Saadeh recalls. The mother had to check her son’s blood glucose levels multiple times during a day using the conventional finger-prick method and administer daily insulin injections.
Most of us who grew up with diabetic parents, grandparents, siblings, or friends are familiar with repeated finger pricking to check sugar levels, which can be painful and also leaves the patient vulnerable to various kinds of infections.
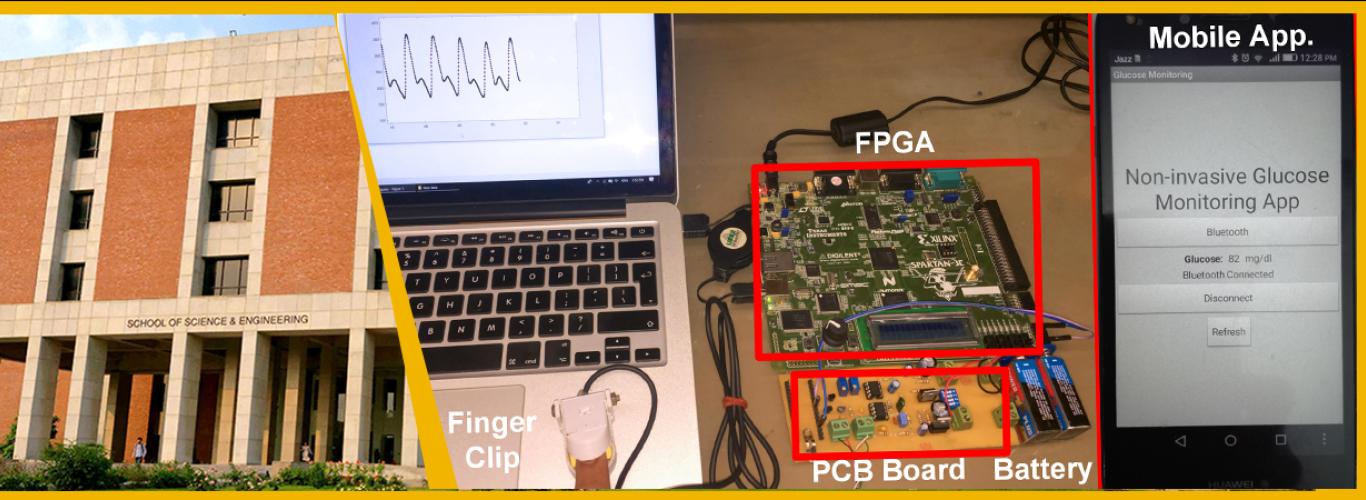
In a research paper co-authored with her student, Aminah Hina, titled, ‘Non-Invasive Glucose Monitoring SoC Based on Single Wavelength Photoplethysmography’ and published in IEEE Transactions on Biomedical Circuits and Systems (Vol. 14, no. 3, pp. 504-515, June 2020), the research team proposes a device such as the ones used in hospitals to monitor the oxygen concentration level and heart rate. The patient basically places his or her finger in a clip-like device, which measures the blood glucose level.
The method involves sending a light wave through the body and detecting glucose levels using a sensor on the other side. Since there is no direct relationship among the incident light, resultant light, and blood glucose level, the team has used a machine learning algorithm trained to map specific light features with certain blood glucose values. The machine learning algorithm allows to detect and quantify glucose levels and is based on a highly sensitive technique for measuring blood volumes using near-infrared optical pulses, called photoplethysmography.
While conducting their research, Dr. Saadeh’s team tested the device on 200 students from LUMS. However, they could not find a sufficient number of diabetic patients on campus. The machine learning algorithm used was therefore calibrated for normal blood glucose levels. They are now working with a local clinic, which treats diabetic patients for recalibrating the algorithm accordingly. The team first demonstrated the initial prototype of the device at the IEEE International Symposium on Circuits and Systems organised in Japan in 2019.
The research team is now working on the second prototype of the device, with the aim of making the circuit smaller to fit onto a single chip and making the measurements even more accurate via extensive testing on diabetic patients.
It is important to note that a few non-invasive blood glucose level monitoring devices such as the GlucoTrack© are available in the market, but are extremely expensive. For example, the one-time cost of GlucoTrack© is approximately PKR 3.4 lac with a recurring cost of PKR 30,000 every 6 months. Once Dr. Saadeh and her team is ready, they aspire to work with companies that manufacture medical devices to make this non-invasive, blood glucose level monitoring device available to the public at affordable rates. Dr. Safeeullah Chaudhry from the School of Science and Engineering’s Biology Department is also closely working with a start-up called Byonyks on non-invasive glucose monitoring. More exciting news is expected to emerge from these groups in due course.
The research paper can be found here.